Understanding Covid-19 and the Vaccine Mandate in the United States
By: Sukhdeep Gill, Karina Peterson, and Jimmy Fang
What is the coronavirus disease?
Coronavirus, also known as Covid-19, is an infectious disease that is caused by the SARS-CoV-2 virus. This virus tends to transmit from small liquid particles from an infected person’s mouth or nose when they cough, sneeze, speak or breathe (CDC, 2021). Most infected people will recover after experiencing mild to moderate symptoms. Those most likely to develop serious illnesses include the elderly and those with underlying medical conditions such as cardiovascular disease, diabetes, chronic respiratory disease, or cancer (CDC, 2021).
Symptoms of Covid-19
According to the Centers of Disease control the following list are symptoms of Covid-19.
- fever
- cough
- tiredness
- loss of taste or smell
- sore throat
- headache
- aches and pains
- diarrhea
- a rash on skin, or discoloration of fingers or toes
- red or irritated eyes
- difficulty breathing or shortness of breath
- loss of speech or mobility, or confusion
- chest pain
How to prevent Covid-19
It is recommended to practice respiratory etiquette, as this virus tends to spread through large to small respiratory droplets. This can be done by practicing the vampire cough in which one coughs in their flexed elbow. Remember to self-isolate for 14 days if positive for Covid-19.
Tips on how to prevent the Coronavirus:
- Stay 6 feet away for others whenever possible
- Wear a fitted surgical mask if N95 isn’t easily accessible
- Get vaccinated as vaccines become available
- Choose open areas with lots of air ventilation over closed areas. Open a window indoors.
- Wash hands regularly with soap and water or alcohol-based hand sanitizers
- Cover mouth and nose when coughing or sneezing
Covid-19 Vaccines
Everyone 5 years of age and older is currently eligible to get vaccinated for Covid-19. There are currently three manufacturers for this vaccine with FDA approval in the United States: Pfizer-BioNTech, Moderna, and Johnson & Johnson’s Janssen (FDA, 2019). Centers for Disease Control does not recommend one vaccine over another (CDC, 2021). All three manufactures currently have a booster available (CDC, 2021).
Pfizer-BioNTech
This vaccine is currently recommended for individuals ages five and older (CDC, 2021). The vaccine is administered in a two-dose series that is given ideally 21 days apart (CDC, 2021). An individual is considered fully vaccinated two weeks after the second dose is administered. A booster is available for everyone ages 18 and older at least six months after the last dose of the series (CDC, 2021). Any of the three vaccines listed can be used as the booster (CDC, 2021).

Moderna
This vaccine is currently recommended for individuals 18 years of age and older and is administered in a two-dose series given 28 days apart (CDC, 2021). An individual is considered fully vaccinated two weeks after the second dose is administered (CDC, 2021). Individuals ages 18 and older are currently eligible for a booster 6 months after the final dose of the series (CDC, 2021). Any of the three vaccines listed can be used as the booster (CDC, 2021).

Johnson & Johnson’s Janssen
This vaccine is currently eligible for all individuals over the age of 18 and is administered in a one dose series (CDC, 2021). An individual is considered fully vaccinated two weeks after receiving the vaccine. Individuals over the age of 18 are eligible for a booster two months after getting the one-dose series vaccine (CDC, 2021). Any of the three vaccines listed can be used as the booster (CDC, 2021).

Vaccine Mandates in the United States
The Biden-Harris administration is requiring all personnel that work in a healthcare facility that participate in the Medicare and Medicaid program to get vaccinated for Covid-19 (CMS, 2021). The administration does offer an exemption to this mandate for qualifying individuals based on a health condition, religious beliefs, observances, or practices. (CMS, 2021). Employers must obtain adequate documentation to justify the exemption. Healthcare Facilities must ensure all eligible staff receive their first dose of a two-dose series vaccine (Moderna and Pfizer) or a one-dose in a One-dose vaccine series (Johnson & Johnson) by December 6, 2022 (CMC, 2021). All eligible staff must be fully vaccinated with either a two-dose or one-dose series by January 4, 2022 (CMS, 2021).
California becomes first state in the Nation that plans to mandate Covid-19 vaccine for schools. Under this mandate students enrolled in in-person learning will be mandated to get vaccinated for Covid-19 starting the term following FDA approval of the vaccine for their grade span (Office of Gavin Newsom, 2021). These grade spans are divided into two categories: k to 6 and 7 to 12. With this mandate all in-person schools will add on Covid-19 vaccination requirements to previously required vaccines such as measles, mumps and rubella (Office of Gavin Newsom, 2021).
Challenges/ Issues/ Reactions to Vaccine Mandate
Although the covid-19 vaccine mandate is a solution to reopening states and cities, the mandate also poses many problems. Prior to the coronavirus pandemic, there has always been high controversy surrounding vaccinations. Many people fear the short-term and long-term effects due to the history of medicine. Others question the amount of time it took to develop the vaccine despite how much technology has grown since past vaccine development. President Joe Biden signed an action plan called “The Path Out of the Pandemic.” causing the workplace to be one of the most affected by the vaccine mandate.
American Airlines was the first to mandate all of their employees to get vaccinated against Covid-19. According to the national public radio report, American Airlines received a great employee response and reported having 99.5% of United employees vaccinated and approximately 2,000 who have applied for religious or medical exemptions in early September (NPR, 2021). In healthcare settings, vaccinations have always been a priority, but the mandate’s response has not been the same. Hospital’s directors and staff members report that the benefit of receiving the vaccine is essential to patients and staff. The Association of American Medical Colleges reports, “In health care, we are called to do amazing work, and part of that calling is a responsibility to keep patients safe; they put their lives in our hands.” Although believed that people will be more willing to take the vaccine on their own after weighing the pros and cons of allowing a self-made decision, a vaccine mandate was deemed more beneficial to most hospitals in America. The mandate comes with losing staff in many workplaces, but perceived benefits of the vaccine show a more negligible risk on the companies.
Healthy People 2030
As we move forward to what is hoped to be the end of a pandemic and settle into our new normal, it is essential to incorporate the covid-19 vaccine and virus into our national goals. One of Healthy People 2030 focuses is preventing infectious diseases by increasing vaccination rates. The covid-19 vaccine development and vaccination mandate will further reduce the number of children who do not receive vaccines, eliminate or minimize coronavirus, and increase the number of adults 19 and above who receive recommended vaccines for preventable diseases. The vaccine mandate will further assist in preventing an infectious disease that brought on a worldwide pandemic.
References
Boyle, Patrick. “Should Hospitals Mandate Covid-19 Vaccination?” AAMC, 15 June 2021,
https://www.aamc.org/news-insights/should-hospitals-mandate-covid-19-vaccination.
California, S. of. (2021, October 1). California becomes First State in nation to announce
COVID-19 vaccine requirements for Schools. Retrieved November 30, 2021, from https://www.gov.ca.gov/2021/10/01/california-becomes-first-state-in-nation-to-announce-covid-19-vaccine-requirements-for-schools/.
Centers for Disease Control and Prevention. (2021). Different covid-19 vaccines. Retrieved
November 30, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines.html.
CMS. (2021, November 4). Press Release Biden-Harris Administration issues emergency
regulation requiring COVID-19 vaccination for health care workers. Retrieved November 30, 2021, from https://www.cms.gov/newsroom/press-releases/biden-harris-administration-issues-emergency-regulation-requiring-covid-19-vaccination-health-care.
DeSilver, D. (2021, October 8). States have mandated vaccinations since long before COVID-19.
Pew Research Center. https://www.pewresearch.org/fact-tank/2021/10/08/states-have-mandated-vaccinations-since-long-before-covid-19/.
Hsu, A. (2021, November 8). Blocked for now, Biden’s vaccine-or-test rule for workers faces
uncertain future Updated November 8, 20219:25 PM ET. NPR. https://choice.npr.org/index.html?origin=https://www.npr.org/2021/11/08/1053625789/blocked-for-now-bidens-vaccine-or-test-rule-for-workers-faces-uncertain-future.
Hsu, Andrea. “Faced with Losing Their Jobs, Even the Most Hesitant Are Getting Vaccinated.”
NPR, NPR, 7 Oct. 2021, https://www.npr.org/2021/10/07/1043332198/employer-vaccine-mandates-success-workers-get-shots-to-keep-jobs.
U.S. Food and Drug Administration. (2021). Covid-19 vaccines. Covid-19 Vaccines. Retrieved
November 30, 2021, from https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines.
World Health Organization. (2021). Coronavirus. Coronavirus disease (COVID-19). Retrieved
November 30, 2021, from https://www.who.int/health-topics/coronavirus#tab=tab_3.
Chronic Pain
By Lori Hayes and Grant Mendoza
Healthy People 2030
Healthy People 2030 has many goals that range from addiction to sexually transmitted infections. The Healthy People 2030 goal that will be the focal point of this health equity blog is chronic pain. The main developmental objectives that will be addressed include, “Increase self-management of chronic pain that frequently limits life or work activities.” Additionally, an objective focused on chronic pain is, “Reduce the impact on loved ones of chronic pain that frequently limits life or work activities.” The last objective that will be addressed in this health equity blog is, “Reduce the proportion of adults with chronic pain that frequently limits life or work activities.” In 2019, 6.9 % of individuals over the age of eighteen had high impacts of chronic pain (Health.gov, n.d.1).
How Do Our Recommendations Address Health Equity?
Our recommendations address health equity because chronic pain is not evenly distributed amongst the population, thus resulting in a health disparity. Individuals develop chronic pain because of an illness or injury that the individual has healed from, but the chronic pain remains constant (John Hopkins Medicine, 2021). Chronic pain can also be caused by arthritis, cancers, headaches, migraines, and neurological disorders (John Hopkins Medicine, 2021). The highest proportion of individuals that suffer from chronic pain include older adults, females, veterans, adults living in poverty (CDC, 2023a).
Due to the high levels of mental health disparities associated with chronic pain, individuals should seek mental health services to aid them in coping with their emotional distresses. In addition, a large health disparity has been identified among individuals having affordable and equitable access to effective pain management care (CDC, 2023a). Out of every twelve adults in the United States, one adult suffers from high-impact chronic pain (Health.gov, n.d.2). Chronic pain has varying durations that can range from weeks to years (Health.gov, n.d.2).
Adult individuals who suffer with chronic pain which effects their daily life and work activities have increased risk of developing depression, Alzheimer’s disease, increased risk of suicide, substance abuse disorders (CDC, 2023a). Additionally, African American and Latinx patients who are of lower socio-economic status suffer from higher rates of uncontrolled chronic pain (CDC, 2022). Thus, reinforcing the desperate need to address the public health issue of chronic pain to improve the quality of life of individuals suffering from the disease. The conditions that individuals are at risk of developing, as well as the suffering from chronic pain reinforces the focus of Healthy People 2030 to reduce the number of individuals suffering with chronic pain. Health education is an essential strategy that will aid in the management of chronic pain.

(Hmccentre, 2023)
Potential Barriers that Lead to Improper Chronic Pain Management
Often, adults who are struggling with chronic pain also struggle with pain management which can result in an opioid addiction (CDC, 2022). To combat the opioid crisis, the CDC developed Opioid Prescribing Guideline which were based on scientific evidence in relation to the public, experts, and was reviewed by the Board of Scientific Counselors (BSC), of the National Center for Injury Prevention and Control which is a federal advisory committee. Multiple system-related health care barriers exist at varying levels such as physician and patient-related that stem which prevent health care professionals from reaching superb pain management (Al-Mahrezi, 2017). A lack of clearly defined standards and pain management protocols as well as limited resources for pain management specialists contribute to the system-related barriers to adequate care (Al-Mahrezi, 2017).
Staff-related barriers which lead to improper chronic pain management include a lack of knowledge and skills pertaining to pain management; lack of knowledge can contribute to false beliefs regarding addiction and overdose (Al-Mahrezi, 2017). Also, patients who seek treatment for chronic pain conditions through an emergency room setting are often treated as a lower priority to other patients (Al-Mahrezi, 2017). All these potential barriers lead to a potential solution which can help individuals struggling with chronic pain management which is education.
Chronic Pain Management Education
Education is a powerful tool which can aid in removing barriers to proper chronic pain management. As a solution, education should be provided to medical professionals as well as patients. Chronic pain management education can be implemented during medical residency programs to help reduce the stigma associated with chronic pain such as opioid addiction. Additionally, education which focuses on prioritizing an updated view of chronic pain management culture will aid in the improvement of health care professional’s pain management skills and attitudes (Al-Mahrezi, 2017).
The holistic approach which includes the mind, body and spirit regarding chronic pain management is a key educational tool which can aide an individual in managing their pain levels. Some holistic approaches to chronic pain management include acupuncture, massage, meditation techniques, music-based interventions, and yoga (Shurleff, 2023). In addition, multiple studies have been conducted on chronic pain management which have been focused on mindfulness-based interventions, including cognitive behavioral therapy (Shurleff, 2023).
Traditionally, chronic pain management was treated with the use of opioids prior to the evidence of addiction the patient experiences was revealed. Today, chronic pain management is treated through nonopioid medications including anticonvulsants, acetaminophen, antidepressants, and specific topical ointments. In addition, chronic pain can be managed through proper exercise, physical therapy, yoga, and nerve blocks. Educating patients who are suffering from chronic pain on alternative treatments that reduce opioid addiction is imperative to reaching the Healthy People 2030 objective.

(Asana, 2022).
References
Al-Mahrezi A. (2017). Towards Effective Pain Management: Breaking the Barriers. Oman
medical journal, 32(5), 357–358. https://doi.org/10.5001/omj.2017.69.
Centers for Disease Control and Prevention. (2022, November 3). CDC Clinical Practice Guideline for prescribing opioids for pain – united states, 2022. Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/71/rr/rr7103a1.htm
Centers for Disease Control and Prevention. (2023a, April 13). Chronic pain among adults – United States, 2019–2021. Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/72/wr/mm7215a1.htm
Chronic pain. Johns Hopkins Medicine. (2021, August 8). https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-pain#:~:text=There%20are%20many%20causes%20of,injury%20or%20evidence%20of%20illness.
Chronic pain management. Headache, Migraine & Concussion Center. (2023, August 30). https://hmccentre.com/chronic-pain-management-ontario/
Health.gov. (n.d.1). Reduce the proportion of adults with chronic pain that frequently limits life or work activities – CP‑01. Reduce the proportion of adults with chronic pain that frequently limits life or work activities – CP‑01 – Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/browse-objectives/chronic-pain/reduce-proportion-adults-chronic-pain-frequently-limits-life-or-work-activities-cp-01
Health.gov. (n.d.2). Chronic pain. Chronic Pain – Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/browse-objectives/chronic-pain#:~:text=Strategies%20to%20help%20people%20manage,adverse%20effects%2C%20including%20opioid%20misuse.
Shurtleff, D. (2023, January). Chronic pain: What you need to know. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/chronic-pain-what-you-need-to-know#:~:text=The%202022%20Centers%20for%20Disease,pain%20conditions%2C%20and%20are%20not
Treating pain without opioids – opioid treatment in Orange County. Asana Recovery. (2022, September 22). https://asanarecovery.com/treating-pain-without-opioids/
Mental Health Among Young Adults
By: Mariana Aldana, Courtney Yang, and Josian Zuniga

Image was taken by: https://pixabay.com/vectors/mental-health-anxiety-depressed-7323725/
Introduction
Mental health is defined as the emotional, psychological, and social-well being of a person (CDC, 2023). In the United States, there are more than 1 in 5 Adults who live with a mental health illness (CDC, 2023). At the National level, about 50% of mental illnesses affect people by age 14 and 75% affect people by the age of 24 (NAMI, n.d.). If mental health problems continue to become prevalent during a person’s early stages of life, it can lead to serious illnesses such as anxiety disorder, bipolar disorder, depression, attention deficit hyperactivity disorder (ADHD), suicide, etc (NAMI, n.d.). When a person experiences a mental health illness, it can affect their ability to think, feel, and act in a healthy manner (CDC, 2023). It can also affect a person’s ability to function effectively on a daily basis. A person’s mental health is equally as important to their physical health (CDC, 2023).
Warning Signs and Symptoms
Prior to receiving a diagnosis, it is important to identify the signs and symptoms of a mental illness. The video, linked here by the National Alliance on Mental Illness, addresses 10 common warning signs of mental health conditions in young adults (NAMI, 2015). To mitigate the risk of mental health issues in the young adult population, it is necessary to be able to identify warning signs and symptoms and utilize preventative methods.
Preventative Methods (Primary, Secondary, and Tertiary Prevention)
Prevention and early intervention strategies can decrease the probability of substance use and mental disorders. Some risk factors for mental health problems can be child maltreatment poverty, and discrimination. Whereas, protective factors include environments that are nurturing, create opportunities, and help with social and emotional skills (Miller et al., 2014). As to mental health promotion, the entire population can be the target. Throughout the individual’s lifespan, making the development and timed achievement of goals much easier are important and necessary in mental health (Min et al., 2013). Assessing the achievement of relevant developmental tasks could be a meaningful topic in mental health promotion and illness prevention (Min et al., 2013).
Under primary prevention, which focuses on many determinants in the whole population or in the high risk group, has three levels of intervention, depending on the risk of the targeted group of individuals (Miller et al., 2014). First, there are universal prevention strategies, which are for example, programs applied in a classroom in order to increase the development of social and emotional skills (Miller et al., 2014). Second, selective prevention programs are for individuals who are at high risk. An example are programs who help increase the resilience of individuals who have parents currently going through a divorce (Miller et al., 2014). Third, coordinated prevention activities target individuals who show indications of an issue, but still do not have the disorder (Miller et al., 2014). For example, the individual is violent.
Secondary prevention, early detection and intervention, aims to support individuals who are to develop mental health problems, due to certain traits of how they were born and/or experiences they have witnessed (Miller et al., 2014). As primary care providers are to screen for possible behavioral health problems, individuals can be provided with care that will help to reduce disorders (Miller et al., 2014). To add on, suicide hotlines and crisis centers also fall under the secondary prevention category because the disorder already exists, but mitigation is possible before the disorder grows rapidly.
Tertiary prevention focuses on the treatment and how the illness/disorder will be managed (Miller et al., 2014). For example, services and outreach can help people with mental illness to be more fully and successfully when participating in their communities, which can then allow them to be positive and accomplish various areas of their lives (Miller et al., 2014). Furthermore, it can include support groups for the loved ones of a patient who has committed suicide to help them heal.
How to Improve Your Mental Health
There are many ways one can improve their mental health, such as staying active, practicing gratitude and relaxation techniques. By staying physically active, it allows individuals to improve the way they think and learn (CDC, 2023). It is recommended that adults do 2 hours and 30 minutes to 5 hours per week of moderate-intensity, or 1 hour and 15 minutes to 2 hours and 30 minutes per week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate and vigorous-intensity aerobic activity (Health, n.d.). Researchers discovered that on average, a person has 3.4 poor mental health days a month. As for those who exercise, the number of poor mental health days decreased by 40% (UCLA Health System, n.d.).
Practicing gratitude, which can be done by jotting down all the things one is grateful for in a journal, can allow one to view life differently. For example, when feeling sad, stressed, or angry, it allows individuals to recognize that they also experience positive moments (U.S. National Library of Medicine, n.d.). Studies have revealed that a single act of thoughtful gratitude can increase happiness by 10% and decrease depressive symptoms by 35% (Angela, 2022).
Relaxation techniques help with the reduction of stress on the mind and body. Some examples of relaxation techniques are visualization, in which one thinks of certain images that take them to a peaceful, calming place (Mayo Clinic, 2022). To accomplish this, using senses such as smell, touch, sound, and sight helps with relaxation. Another technique is muscle relaxation, where muscles slowly tense up and then become relaxed (Mayo Clinic, 2022). This specific technique allows individuals to be more conscious of physical sensations.

Image was taken by: https://pixabay.com/vectors/yoga-zen-meditation-position-relax-304635/
Mental Health Resources
If identifying the signs and symptoms and practicing preventative methods do not help lower the risk of a person’s mental health, the next best step is to utilize mental health resources to connect with mental health professionals. Listed below are some resources specifically catered to Mental Health. To access these mental health resources, please visit here. (NAMI, n.d.b).
- 988 Suicide & Crisis Lifeline
- NAMI Teen & Young Adult (T&YA) Helpline
- NAMI Helpline
Healthy People 2030 and Young Adult Mental Health
As with most public health issues, it is essential to be collectively aligned in efforts and strategies to address mental health in young adults. National health objectives, like those from Healthy People 2030, provide standardized health objectives for public health professionals and health educators to incorporate into their health programs/curriculum. One of the Healthy People 2030 Leading Health Indicators (LHIs) is to increase the proportion of adolescents (ages 12-17) with depression who get treatment (Office of Disease Prevention and Health Promotion, 2020). An LHI is a subset of high priority Healthy People 2030 objectives. Unfortunately, this objective currently has little to no detectable change (Office of Disease Prevention and Health Promotion, 2020). When developing new programs that address mental health, objectives such as this one must be at the forefront of design to ensure that health professionals are supporting priority populations. The aforementioned prevention strategies provide activities and tools to easily incorporate into health programs while staying consistent with Healthy People 2030 objectives.
A primary root cause of mental health concerns among young adults and adolescents arise from trauma. There has been a recent trend in shifting mental health conversations to recognizing and responding to symptoms of trauma (Marris, 2022). This is known as trauma-informed care (TIC). Healthy People 2030 also highlights this emerging need as seen in the objective that aims to increase the proportion of adolescents with symptoms of trauma who get treatment (Office of Disease Prevention and Health Promotion, 2020). Cross-sector collaboration is necessary to mitigate the effects of trauma and to foster healing from a mental health perspective. These efforts occur across all levels of prevention, from developing multifaceted mental health curriculum in schools to implementing appropriate care management programs for adolescents and young adults experiencing trauma-related mental health issues.
Conclusion
Mental health in adolescents and young adults is an increasingly growing concern in the United States that involves a complex variety of health determinants. Emphasizing methods to detect mental health early and promoting proper diagnosis is essential to addressing mental health. These efforts require the collaboration of varying levels of prevention that ranges from self-awareness to school programs to targeted interventions. However, it is equally important that participating actors are equipped with emerging resources and education (i.e., trauma-informed care) to combat these issues. Disseminating relevant and accessible interventions, activities (such as showing gratitude, staying active, and relaxation), and resources (such as mental health helplines) will also help fortify mental health programs. By centering local and national efforts around Healthy People 2030 objectives it will help close this gap and ensure the health of our future generations.
References
Angela. (2022). The importance of practicing gratitude and celebrating small victories. Mental Health First Aid. https://www.mentalhealthfirstaid.org/2022/11/practicing-gratitude/#:~:text=Research%20has%20shown%20that%20consciously,35%25%20reduction%20in%20depressive%20symptoms.
Centers for Disease Control and Prevention. (2023). About Mental Health. https://www.cdc.gov/mentalhealth/learn/index.htm
Centers for Disease Control and Prevention. (2023). Benefits of physical activity. Centers for Disease Control and Prevention. https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm#:~:text=Regular%20physical%20activity%20can%20help,and%20help%20you%20sleep%20better.
Mayo Foundation for Medical Education and Research. (2022). Relaxation techniques: Try these steps to reduce stress. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/relaxation-technique/art-20045368#:~:text=It’s%20a%20process%20that%20decreases,as%20heart%20disease%20and%20pain.
Miller, J., Gordon, S., & Shea, P. (2014). Reducing the Burden of Mental Illness: The Role of Preventive Activities and Public Health Strategies. National Association of State Mental Health Program Directors. https://www.NASMHPD, 2014.org/sites/default/files/2022-08/Prevention%2520Issue%2520Brief%2520-%25209-23-14%2520FINAL.pdf
Min, J.-A., Lee, C.-U., & Lee, C. (2013). Mental Health Promotion and Illness Prevention: A Challenge for Psychiatrists. Psychiatry investigation. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3902147/#:~:text=THE%20CONCEPTS,-Health%20promotion%20mainly&text=There%20are%20three%20categories%20of,and%20reduction%20of%20relapse%20risk.
National Alliance on Mental Illness (NAMI). (n.d.). Mental Health Conditions. https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions
National Institute of Mental Health (NIH). (n.d.). NAMI Helpline. https://www.nami.org/help
National Alliance on Mental Illness (NAMI). (2015). 10 Common Warning Signs of A Mental Health Condition [Video]. YouTube. https://www.youtube.com/watch?v=zt4sOjWwV3M&t=2s
Office of Disease Prevention and Health Promotion. (2020). Increase the proportion of adolescents with depression who get treatment — MHMD‑06 https://health.gov/healthypeople/objectives-and-data/browse-objectives/mental-health-and-mental-disorders/increase-proportion-adolescents-depression-who-get-treatment-mhmd-06
Office of Disease Prevention and Health Promotion. (2020). Increase the proportion of primary care visits where adolescents and adults are screened for depression — MHMD‑08 https://health.gov/healthypeople/objectives-and-data/browse-objectives/mental-health-and-mental-disorders/increase-proportion-primary-care-visits-where-adolescents-and-adults-are-screened-depression-mhmd-08
Office of Disease Prevention and Health Promotion (OASH). (n.d). Current Guidelines. ttps://health.gov/our-work/nutrition-physical-activity/physical-activity-guidelines/current-guidelines
SAMHSA. (n.d.).Prevention of Substance Use and Mental Disorders. https://www.samhsa.gov/find-help/prevention
UCLA Health System. (n.d.). The Link Between Exercise and Mental Health. https://www.uclahealth.org/news/the-link-between-exercise-and-mental-health#:~:text=Physical%20activity%20improves%20mental%20health&text=Researchers%20found%20that%2C%20on%20average,by%20more%20than%2040%20percent
U.S. National Library of Medicine. (n.d.). How to Improve Mental Health. MedlinePlus. https://medlineplus.gov/howtoimprovementalhealth.html
Preserving Your Smile: Strategies for Adult Tooth Decay Prevention
By Dilpreet Sekhon and Hermelinda Guzman
Dental cavities, also known as dental caries or tooth decay, are a common dental issue characterized by the demineralization and destruction of tooth enamel and underlying structures ((National Institute of Dental and Craniofacial Research, 2018). Cavities are caused by many factors, primarily involving bacteria, diet, and oral hygiene (NIDCR, 2018). Dental caries (tooth decay or cavities) remains the most prevalent chronic disease in children and adults, even though it is preventable (NIDCR 2018). Cavities are an unmet treatment need that can cause deterioration if not attended to early (CDC, 2021). According to the Global Burden of Disease Study 2019, dental and oral health issues, particularly dental caries, affect half of the global population, equating to approximately 3.58 billion people. Untreated tooth decay can affect essential aspects of daily living, including eating, speaking, and performing at home, school, or work (Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, 2021). The Healthy People 2030 aims to reduce the proportion of adults with active or untreated tooth decay from 22.8 percent to 17.3 percent. This is among adults aged 20-74 years of age (Office of Disease Prevention and Health Promotion (OASH), n.d.).
How Common is Toothy Decay in Adults
It is estimated that around 90% of adults ages 20 years or older have had at least one cavity (CDC, 2023). Approximately 25% of adults aged 20 to 64 currently have at least one cavity (CDC, 2023). In older adults, periodontal disease occurs in 7 out of 10 older adults, with untreated tooth decay occurring in 1 out of 5 adults (Kwon et al., 2021). 1 in 4 adults have lost a large proportion of their teeth (Kwon et al., 2021). Nelson and associates (2020) note that senior citizens from minority and low-income backgrounds tend to experience untreated tooth decay at a higher rate.

Importance of Improving Oral Health
Improving oral health is necessary due to the impact on the quality of life of an individual. Oral health in America has drastically improved within the last century; and although many populations have access to preventative and restorative dental care, there is still a large number of oral health inequalities among vulnerable and underserved communities (Northridge et al., 2020). Barriers such as access to dental care, high costs, lack of oral health literacy, and emergency room visits continue to affect uninsured individuals, low income and rural populations, and other disadvantaged minorities (Northridge et al., 2020). Oral diseases can significantly impact people’s lives, causing trouble with chewing, and reduced food intake leading to weight loss, sleep problems, irritability, and low self-esteem (Spanemberg et al., 2019). Additionally, disorders such as malocclusion, tooth eruption issues, dental trauma, mouth tissue tumors, clefts in lips and palate, and tooth stains (such as dental fluorosis) may also affect some individuals with varying frequency (Spanemberg et al., 2019). Unfortunately, limited information is available on these conditions’ potential functional, emotional, and social consequences (Spanemberg et al., 2019).
Oral Health Disparities
Inadequate oral health outcomes result from poor oral health literacy, which is especially common among older adults. Kwon and associates (2022) note that around 56.9% of the elderly have insufficient oral health knowledge, with those over 75 years of age being affected more. Older adults with a lower socioeconomic status were significantly associated with poor oral health knowledge (Kwon et al., 2022). The ethnicities more likely affected by this disparity were Asians and Hispanics with them 2.5 more times and 25 more times likely to report insufficient oral health knowledge, respectively (Kwon et al., 2022).
Healthy Living Tips
Water Fluoridation
One of the best preventative measures is the fluoridation of water (Northridge et al., 2020). Fluoridation can inhibit bacterial activity in dental plaque and reduce enamel demineralization when acid is present in the mouth cavity (Pollick, 2018). This acid is present during the breakdown of carbohydrates and the correct dosage and concentration of fluoride significantly impacts the oral health of a community (Pollick, 2018). The infographic to the right on tooth decay prevention recommends brushing your teeth daily at least twice with fluoridated toothpaste (Toh, 2022).

Proper Cleaning
It is important to brush the teeth two times a day using fluoride toothpaste and to make sure that toothpaste does not get swallowed frequently since it can lead to fluorosis (National Institute of Dental and Craniofacial Research, 2022). Daily flossing at least once a day and an antibacterial mouthwash are recommended (CDC, 2023). Proper brushing and flossing are an essential tool in preventing cavities, however, many people are unaware of how to do it correctly. Below is the proper way to brush and floss, once achieved, it should be a fast and easy technique.

Healthy Diet
It’s important to consume a variety of foods that provide the necessary nutrients and to limit the intake of sugary and acidic items to prevent dental issues and support your overall well-being (Jayasinghe et al., 2022). According to Jayasinghe and associates (2022), there is a bi-directional link between nutrition and oral health, in that nutrition affects the health of oral tissues and saliva, and the health of the mouth may affect the foods consumed. It is essential to reduce frequent snacking so the teeth can repair themselves from frequent acid attacks (NIDCR, 2022). Fruit juice and foods with sugar and starches should be limited, especially after bedtime brushing. The infographic above provides a detailed list of foods to avoid.
Visiting the Dentist
Regular dentist visits could prevent the deterioration of tooth decay especially when caught early (NIDCR, 2022). It is crucial to visit the dentist at least once a year (CDC, 2023). The dentist could remove dental plaque and check for early tooth decay in any area (NIDCR, 2022). If there are any symptoms of tooth pain, swelling, changes in taste, smell, or tooth sensitivity, it is best to schedule an appointment with the dentist (CDC, 2023)
Summary
In conclusion, the high occurrence of tooth decay among adults poses a significant public health concern, impacting the overall well-being, and quality of life of individuals. Tooth decay, although preventable, continues to affect a significant portion of the adult population, leading to various health issues and disparities, especially among older adults, low-income individuals, and certain ethnic groups. A crucial step toward improving oral health and achieving health equity is the Healthy People 2030 initiative, which aims to reduce the proportion of adults with untreated tooth decay. A multi-faceted approach is necessary for preserving one’s smile and enhancing oral health. Water fluoridation, which experts recommend, plays a vital role in preventing tooth decay, inhibiting bacterial activity, and protecting enamel. Regular dental check-ups and proper cleaning habits are essential for maintaining good oral health. These strategies help address oral health disparities by providing accessible and effective preventive care for all, regardless of age, income, or ethnicity, and contribute to the achievement of Healthy People 2030 goals. In a society that increasingly recognizes the importance of holistic well-being, it is imperative to prioritize oral health as an integral part of overall health equity, ensuring that everyone can preserve their smiles and lead healthier lives.
References
Broomhead, T., Ballas, D., & Baker, S. (2021). Neighborhoods and oral health: Agent-based modelling of tooth decay. Health & Place, 71, 102657. https://doi.org/10.1016/j.healthplace.2021.102657
Center for Disease Control and Prevention. (2021, January 25). Cavities. https://www.cdc.gov/oralhealth/fast-facts/cavities/index.html
Center for Disease Control and Prevention (CDC). (2023, April 10). Oral Health Tips. Center for Disease Control and Prevention. https://www.cdc.gov/oralhealth/basics/adult-oral-health/tips.html
Elegant Dental Care. (2020, January 14). How to floss your teeth (Complete guide). Elegant Dental Care. https://www.elegantdentcare.com/blog/how-to-floss-your-teeth-complete-guide/
Horst, J. A., Tanzer, J. M., & Milgrom, P. M. (2018). Fluorides and Other Preventive Strategies for Tooth Decay. Dental Clinics of North America, 62(2), 207. https://doi.org/10.1016/j.cden.2017.11.003
Jayasinghe, T. N., Harrass, S., Erdrich, S., King, S., & Eberhard, J. (2022). Protein Intake and Oral Health in Older Adults-A Narrative Review. Nutrients, 14(21), 4478. https://doi.org/10.3390/nu14214478
Kabir Post. (2018, March 5). Top 10 Ways to a Better Dental health. https://kabirpost.com/top-10-ways-better-dental-health/
Kwon, S. R., Lee, S., Oyoyo, U., Wiafe, S., Guia, S. D., Pedersen, C., Martinez, K., Rivas, J., Chavez, D., & Rogers, T. (2021). Oral health knowledge and oral health related quality of life of older adults. Clinical and Experimental Dental Research, 7(2), 211-218. https://doi.org/10.1002/cre2.350
National Institute of Dental and Craniofacial Research (NIDCR). (2018). Dental Caries (Tooth Decay). Retrieved from https://www.nidcr.nih.gov/research/data-statistics/dental-caries
National Institute of Dental and Craniofacial Research (NIDCR). (2022, August). The tooth decay process: How to reverse it and avoid a cavity. https://www.nidcr.nih.gov/health-info/tooth-decay/more-info/tooth-decay-process
Nelson, S., Albert, J. M., & Milgrom, P. (2020). Comparative Effectiveness of Two Nonsurgical Treatments to Reduce Oral Health Disparities From Untreated Tooth Decay in Older Adults: Protocol for a Cluster Randomized Trial. JMIR research protocols, 9(9), e17840. https://doi.org/10.2196/17840
Northridge, M. E., Kumar, A., & Kaur, R. (2020). Disparities in Access to Oral Health Care. https://doi.org/10.1146/annurev-publhealth-040119-094318
Office of Disease Prevention and Health Promotion [OASH]. (n.d.). Reduce the proportion of adults with active or untreated tooth decay — OH‑03 – Healthy People 2030https://health.gov/healthypeople/objectives-and-data/browse-objectives/oral-conditions/reduce-proportion-adults-active-or-untreated-tooth-decay-oh-03
Pollick, H. (2018). The Role of Fluoride in the Prevention of Tooth Decay. Pediatric Clinics of North America, 65(5), 923-940. https://doi.org/10.1016/j.pcl.2018.05.014
Spanemberg, J., Cardoso, J., Slob, E., & López-López, J. (2019). Quality of life related to oral health and its impact in adults. Journal of Stomatology, Oral and Maxillofacial Surgery, 120(3), 234-239. https://doi.org/10.1016/j.jormas.2019.02.004
Living Healthy With Hypertension
By Lori Hayes and Grant Mendoza

Healthy People 2030
Two distinct Healthy People 2030 objectives deal with hypertension prevalence and management. The first Healthy People 2030 goal is to “reduce the proportion of adults with high blood pressure – HDS-04”. The second goal is to “Increase control of high blood pressure in adults – HDS-05” (Office of Disease Prevention and Health Promotion, n.d.).
Barriers to Hypertension Awareness, Treatment, and Control

Figure 2: Stock Photo of an individual getting their blood pressure measured by a health professional.
Hypertension and Access to Healthcare
Two studies investigated access to healthcare and hypertension prevalence, awareness, treatment, and control. In the first study, conducted in China between 1989 and 2011, Yang and colleagues (2018) analyzed data from participants aged 18 years and older who had their blood pressure taken during the examination. The researchers found that hypertension prevalence increased non-linearly with age within a given cohort and was higher in succeeding cohorts compared to older ones (Yang et al., 2018). The study also revealed that hypertension prevalence was higher among males and individuals with insurance (Yang et al., 2018). The researchers attributed this finding to a lack of physical activity and rising childhood obesity, which could be contributing to the increasing prevalence of hypertension. The study suggested that having insurance could increase access to healthcare, leading to higher hypertension prevalence among those insured (Yang et al., 2018).
In the second study, conducted in Cheonan, Korea, in 2017, they analyzed data from the 2010-2013 Korea National Health and Nutritional Examination Survey, which had a total of 20,044 participants aged 30 years and older (Lee, 2018). They found that Korea had a higher level of unawareness of hypertension compared to the United States or Canada. The study suggested that this difference may be due to socioeconomic status, health behaviors, and accessibility to healthcare (Lee, 2018). Overall, these studies shed light on the disparities in hypertension prevalence, awareness, treatment, and control and could help inform future interventions to reduce these disparities.
Hypertension and Food Deserts
Testa and colleagues (2021) conducted a study that examined how food deserts affect cardiovascular health and how socioeconomic status acts as a buffer in this context. The researchers suggested that food deserts can influence cardiovascular health in three ways:
- Residents of food deserts often make food choices based on local availability, and since food deserts are typically characterized by a lack of healthy food options, residents usually end up consuming high-energy, non-nutritious foods.
- Residing in a food desert can increase the amount of time that residents have to spend obtaining healthier food options, resulting in less time for physical exercise or leisure time.
- Residents who live in food deserts may be more economically deprived than those who do not, which can increase the risk of cardiovascular diseases (Testa et al., 2021).
Garg and colleagues (2023) investigated the association between neighborhood food environments and the risk of incident hypertension using electronic health record data from health centers across Chicago and zip-code supermarket access. The study hypothesized that the greater the average distance to the supermarket, the higher the risk of developing hypertension (Garg et al., 2023). The researchers found a significant association between neighborhood food environments and incident hypertension, with those living farther away from supermarkets at a higher risk of developing hypertension (Garg et al., 2023). The study highlights the importance of access to healthy food options in reducing the risk of developing hypertension.
Recommendations and Programs to Reduce Hypertension

Figure 3: Stock Photo of individuals exercising in a group setting.
Nonpharmacological Treatment of Hypertension
For individuals with elevated blood pressure or mild hypertension, nonpharmacological interventions may be helpful in the prevention of stage 1 or 2 hypertension. These nonpharmacological interventions include weight loss, increasing physical activity, and a healthy diet emphasizing sodium reduction (Whelton et al., 2018). Weight loss is the most significant factor when considering lowering blood pressure. Weight loss should be coupled with increased physical activity and reduced dietary sodium intake. The American College of Cardiology guidelines provide approximate impacts of the interventions on systolic blood pressure. Weight loss is the first mentioned intervention. They claim that an individual should expect the systolic blood pressure to drop about one mmHg per 1 kg of body weight lost (Whelton et al., 2018). The most impactful nonpharmacological intervention was the DASH diet, which provided an approximate drop of 11 mmHg in systolic blood pressure (Whelton et al., 2018). Increasing physical aerobic activity is the second most impactful intervention in reducing systolic blood pressure. The guideline suggests that 90-150 minutes of aerobic exercise per week can reduce approximately eight mmHg of systolic blood pressure (Whelton et al., 2018). Sodium reduction is the third most impactful intervention, providing a drop of about six mmHg of systolic blood pressure in individuals with hypertension but only a drop of 2 mmHg of systolic blood pressure in individuals with normal blood pressure (Whelton et al., 2018).
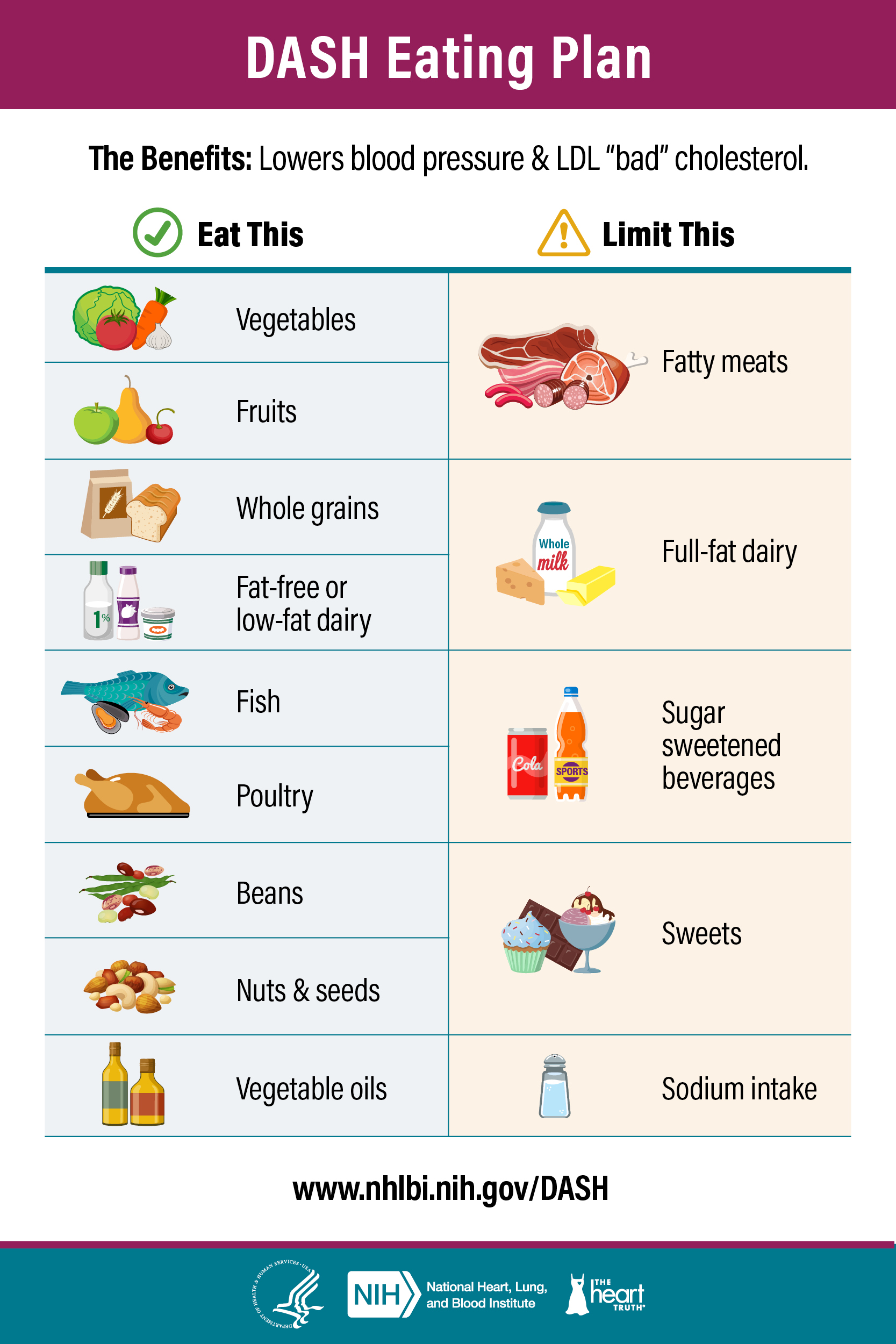
The DASH Diet
The Dietary Approaches to Stop Hypertension (DASH) is a diet plan focusing on consuming fruits, vegetables, and low-fat dairy products. Evidence supports decreased systolic and diastolic pressures (Juraschek et al., 2018). The DASH-sodium trial showed that reducing sodium will decrease blood pressure independently of the effects of the DASH diet.
Hypertension Control Course
Harvard University offers an online course named Controlling your Blood Pressure that is aimed at providing students with the resources to manage their blood pressure at home. The course is $30, but it is online and available anytime. There is a time commitment of 2-4 hours a week, but the course is self-paced, so there is no stress to make deadlines. This course is led by Harvard faculty as they share strategies to understand the causes of hypertension and how to use today’s advancements to manage hypertension. The only limitation of this course is that it is only offered in English.
Link to the course: https://pll.harvard.edu/course/controlling-your-blood-pressure

Figure 5: Importance of blood pressure control in Spanish. This picture discusses the activities that individuals can perform, the systolic pressure points reductions, and the significance of the blood pressure reductions. This was taken from Million Hearts, CDC.
Summary
There are two Healthy People 2030 objectives that aim to combat hypertension in the United States. The first is reducing hypertension prevalence, and the other is increasing the percentage of individuals with controlled hypertension. There are multiple barriers to hypertension awareness, treatment, and control. Food deserts and access to healthcare are two major barriers that affect individuals with hypertension. Recommendations to improve hypertension awareness, treatment, and control include weight loss, increased physical activity, and a healthy diet. Harvard University offers a hypertension control course for individuals looking for resources and guidance on managing their blood pressure.
References
Garg, G., Tedla, Y. G., Ghosh, A. S., Mohottige, D., Kolak, M., Wolf, M., & Kho, A. (2023). Supermarket Proximity and Risk of Hypertension, Diabetes, and CKD: A Retrospective Cohort Study. American Journal of Kidney Diseases, 81(2), 168–178. https://doi.org/10.1053/j.ajkd.2022.07.008
Juraschek, S. P., Miller, E. R., Weaver, C. M., & Appel, L. J. (2018). Effects of Sodium Reduction and the DASH Diet in Relation to Baseline Blood Pressure. Journal of the American College of Cardiology, 70(23), 2841–2848. https://doi.org/10.1016/j.jacc.2018.10.011
Lee, H.-Y. (2018). Socioeconomic Disparities in the Prevalence, Diagnosis, and Control of Hypertension in the Context of a Universal Health Insurance System. Journal of Korean Medical Science, 32(4), 561. https://doi.org/10.3346/jkms.2018.32.4.561
Office of Disease Prevention and Health Promotion. (n.d.). Heart Disease and Stroke. Healthy People 2030 U.S. Department of Health and Human Services. Retrieved October 18, 2023, from https://health.gov/healthypeople/objectives-and-data/browse-objectives/heart-disease-and-stroke
Testa, A., Jackson, D. B., Semenza, D. C., & Vaughn, M. G. (2021). Food deserts and cardiovascular health among young adults. Public Health Nutrition, 24(1), 117–124. https://doi.org/10.1017/S1368980020001536
Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E., Collins, K. J., Dennison Himmelfarb, C., DePalma, S. M., Gidding, S., Jamerson, K. A., Jones, D. W., MacLaughlin, E. J., Muntner, P., Ovbiagele, B., Smith, S. C., Spencer, C. C., Stafford, R. S., Taler, S. J., Thomas, R. J., Williams, K. A., … Wright, J. T. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Journal of the American College of Cardiology, 71(19), e127–e248. https://doi.org/10.1016/j.jacc.2017.11.006
Yang, F., Qian, D., & Liu, X. (2018). Socioeconomic disparities in prevalence, awareness, treatment, and control of hypertension over the life course in China. International Journal for Equity in Health, 16(1), 100. https://doi.org/10.1186/s14939-017-0597-8
Diabetes Self-Management Education
By Lori Hayes and Grant Mendoza
Healthy People 2030
One of Healthy People 2030’s goals is to” Reduce the burden of diabetes and improve quality of life for all people who have, or are at risk for, diabetes.” Another Healthy People 2030 goal that addresses diabetes education states, “Increase the proportion of people with diabetes who get formal diabetes education.” Formal diabetes education assists the individual with the proper knowledge, skills, and abilities needed to manage their disease. Diabetes education focusing on nutrition and physical activity is essential to decreasing the incidence rate of diabetes.
Recommendations to Address Health Equity
Our recommendations address health equity because the Latinx population is disproportionately affected by diabetes and, therefore, needs education intervention so the population can reach the highest level of health. Seventeen percent of Latinx individuals are likely to develop type 2 diabetes compared to eight percent of non-Hispanic white individuals (CDCa, 2022). Providing health education regarding diabetes self-management education to the Latinx population that is culturally appropriate is a mechanism to reduce the condition’s prevalence.
The Latinx population is also more likely to suffer from diabetes-related conditions more severely in comparison to non-Hispanic individuals. These conditions stemming from diabetes include kidney failure, diabetic retinopathy, and the complete loss of vision abilities (CDCa, 2022). Because Latinx individuals are twice as likely to be diagnosed with type 2 diabetes in comparison to non-Hispanic whites, they are also at an increased risk of morbidity or mortality (Liburd et al., 2019). These extreme conditions reinforce the importance of diabetes management and working towards healthy equity in the Healthy People 2030 goals.

(Gourlay, 2016).
Barriers that Lead to Improper Diabetes Management
Often, individuals are diagnosed with diabetes, but they lack the proper foundation needed to help manage and control their disease. Additional barriers need to be addressed, including communication and culture within the doctor’s office. Latinx individuals who are diagnosed with diabetes and who cannot talk effectively with their doctor are much less likely to follow through with their treatment regimen (CDCa, 2022). Ineffective communication between the patient and the doctor can result in the patient misusing their medication. This can result in the patient receiving the incorrect amount of insulin, which can lead to adverse effects.
Culture plays a prominent role in the development of diabetes among Latinx individuals due to individuals placing their personal needs last and their family member’s needs first (CDCa, 2022). Also, if Latinx individuals do not form a secure and trustworthy relationship with their doctor, they are more likely to utilize traditional medicine instead of the standard diabetes medication prescribed by doctors (CDCa, 2022). Latinx individuals who live below the federal poverty level and have a low educational attainment level are more susceptible to having poor glycemic control (Liburd et al., 2019).
Diabetes Self-Management Education and Support
Diabetes self-management education and support (DSMES) assists individuals with type 2 diabetes in managing their condition and can be tailored to the individual’s life (CDCb, 2022). Diabetes self-management education (DSME) focuses on the skills, knowledge, and attitudes that are necessary for type 2 diabetic individuals to manage their chronic conditions effectively. DSME has been proven to be effective in positive lifestyle changes and improved self-care in patients with type 2 diabetes (Ernawati et al. 2021). Once type 2 diabetic patients have the proper skills and information, they need to manage their condition, their monitoring of glucose levels improves; self-efficacy plays an influential role in this improvement (Ernawati et al., 2021).
The components of DSME classes include how to utilize your glucose monitor to get an accurate reading, proper nutrition, the necessary physical education, how to manage the significant stressors in life, and how to take prescribed medications as instructed (CDCc, 2018). In addition to the information provided to the DSME participants, they also gain a sense of community and support by participating in the program. The proper type 2 diabetes nutrition includes eating a balanced diet that is low in simple carbohydrates, sugars, and fats and high in protein and fiber. Also, engaging in at least thirty minutes of physical activity every day can assist type 2 diabetic individuals in regulating their sugar levels and decreasing their sedentary lifestyle. In conclusion, by adding these lifestyle modifications to your everyday activities, you can help reduce your A1c1 levels and live a high quality life.
References
Centers for Disease Control and Prevention. (2022a, April 4). Hispanic or Latino people and type 2 diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html#:~:text=Each%20has%20its%20own%20history,is%20closely%20tied%20to%20background.
Centers for Disease Control and Prevention. (2022b, November 3). Education and support. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/managing/education.html
Centers for Disease Control and Prevention. (2018c, December 18). Managing diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/learnmorefeelbetter/programs/diabetes.htm
Centers for Disease Control and Prevention. (2023d, July 18). Diabetes self-management education and support (DSMES) toolkit. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/dsmes-toolkit/index.html
Ernawati, U., Wihastuti, T. A., & Utami, Y. W. (2021, April 14). Effectiveness of diabetes self-management education (DSME) in type 2 diabetes mellitus (T2DM) patients: Systematic Literature Review. Journal of public health research. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8129774/
Gourlay, K. (2016, August 11). Exploring disparities in diabetes among Latinos. Exploring Disparities in Diabetes Among Latinos. https://centerforhealthjournalism.org/our-work/insights/exploring-disparities-diabetes-among-latinos
Liburd, L. C., Chrvala, C. A., Carbone, E. T., Mansyur, C. L., Sarkar, U., Snoek, F., Bouton, M. E., Beckles, G. L., Benjamin, E. J., Chandler, R. F., Beck, J., Laiteerapong, N., Chamberlain, J. J., Khunti, K., Marrero, D. G., Powers, M. A., Li, R., Ada, Chen, R., … Israel, H. (2019, September 9). Effect of diabetes self-management education on glycemic control in Latino adults with type 2 diabetes: A systematic review and meta-analysis. Patient Education and Counseling. https://www.sciencedirect.com/science/article/abs/pii/S073839911930415X
Empowering Women’s Health: Promoting Breast Cancer Screening Amongst Older Women
By Dilpreet Sekhon and Hermelinda Guzman
How Common is Breast Cancer?
Within the United States, breast cancer is the most prevalent cancer diagnosis and is the second most prominent cause of mortality among women (CDC, 2022). Breast cancer affects 1 in 8 women in the United States, and only around 20% of cases are due to genetic factors (Britt et al., 2020). Around 75.6% of the female population gets screened for breast cancer. Healthy People 2030 aims to increase the percentage of women aged 50-74 getting screened to 80.5% (Office of Disease Prevention and Health Promotion [OASH], n.d.). Breast cancer screening is crucial, and early screening and lifestyle changes can create a healthy lifestyle for older women.

Importance of Screening
According to the United States Preventive Services Task Force (USPSTF), mammogram screenings for women aged 50-59 could potentially lead to a reduction of 7.7 deaths per 10,000 women, and for those aged 60-69, the reduction could be as high as 21.3 deaths per 10,000 women (Hathaway et al., 2021). Women who underwent screening mammograms had a 21% lower likelihood of receiving later-stage diagnoses than those who did not (Hathaway et al., 2021).
In a study conducted by Pitman and his colleagues in 2017, an examination was made into the impact of adhering to breast cancer screening guidelines on breast cancer incidence rates among two age groups: women aged 40-44 and 45-59 (Pitman et al., 2017). The study findings revealed that if women aged 40-45 followed the American Cancer Society’s (ACS) recommendations for screening before the age of 45, there would be an 8.9% reduction in missed breast cancer diagnoses (Pitman et al., 2017). Conversely, if women aged 40-49 adhered to the recommendation of waiting until age 50 for their routine mammograms, it would result in an 18.8% increase in breast cancer diagnoses (Pitman et al., 2017).
Tips for Healthy Living
Understanding USPSTF Guidelines
The USPSTF guidelines have been modified since 2009 for women aged 40 and older. Biennial screenings are recommended for women aged 50-74; however, screening for women younger than 50 should depend on their risk factors and family history (Brown et al., 2018). Before, the guidelines indicated that women obtain screenings every 1-2 years, and patient’s perceptions about the harms or benefits of mammograms were not accounted for (Brown et al., 2018). The current guidelines for women aged 75 years and older do not have enough evidence to support for or against screening (Brown et al., 2018).
Family History
If an individual has a first-degree or second-degree relative with breast cancer, they have an increased risk of developing breast cancer (Li et al., 2018). It is important to evaluate who has breast cancer in the family and share with the primary care physician for more advice on screening and obtaining referrals for a mammogram. The graphic shows the four family history patterns that are red flags that an individual should look out for.

Maintaining a Healthy Lifestyle
Physical activity at a moderate or vigorous level is crucial. It can help reduce the relative risk of breast cancer by 20% when compared independent of body mass index (BMI), another mediating factor (Britt et al., 2020). It is essential to be active and limit alcohol consumption. The Nurses’ Health Study highlighted that those who consume 30g of alcohol daily have an increased risk of developing breast cancer by 50% compared to the increased risk of 15% among women who consume 5-10 g of alcohol daily (Britt et al., 2020). The infographic shows the ways women can live a healthier lifestyle by being active and limiting alcohol consumption.
Increasing the number of breast cancer screenings
Reduce your risk
Given the importance of breast cancer screenings, early diagnosis is one measure to reduce breast cancer deaths; therefore, women must get screened and utilize breast screening programs. According to Laszlo Tabar and associates (2015), women should be informed that early breast cancer detection with mammography is associated with a significantly reduced risk of being diagnosed with advanced breast cancer and dying from breast cancer. Women should also be informed of the importance of adhering to a regular screening schedule to ensure the greatest likelihood of having growing breast cancer detected. At the same time, it is still small and localized to the breast, and the

limitations and harms associated with breast cancer screening (Smith et al., 2014).
One approach to early detection is to become aware of the signs and symptoms, which can start at home; however, it is based on a woman’s perception and understanding of breast self-exams, clinical exams, and mammograms. The infographics show the four things to look for during a breast self-exam and how mammograms can detect smaller breast lumps earlier.
Many factors, including inadequate training on breast self-exams, lack of awareness, fear, and negative attitudes toward findings can control these perceptions.

Source: Singapore Cancer Society, n.d.
Limiting Barriers
Another way to increase breast cancer screenings is to provide access to services. Many minority populations face barriers when it comes to accessing healthcare. For instance, transportation issues, lack of economic and educational resources, provider shortages, and limited healthcare coverage (Lee et al., 2015). Ensuring care through grant-funded interventions, low-cost or no-cost services, health education, and advocating for policy change can increase awareness and limit access disparities. This addresses health equity since it ensures that barriers to screening are addressed, and women have access to mammograms regardless of their socioeconomic status or language barriers.
Conclusion
Getting preventive care reduces the risk late-stage diagnoses for breast cancer and early detection can start from home through self-exams. Acquiring preventive measures for breast cancer are crucial because they not only save lives and reduce occurrence but also contribute to the overall well-being of individuals and communities. By focusing on prevention, societies can begin to build healthier, long-lasting futures. Although more women are getting screened, the Healthy People 2030 objective is to increase the proportion of women getting screened. Early detection is crucial in improving outcomes and reducing health disparities alongside a comprehensive approach to women’s health that encompasses regular screenings, a healthy lifestyle, and the empowering practice of breast self-exams amongst older women.
References
AdventHealth Florida. (2018, November 13). Reduce Your Breast Cancer Risk – Tip #7 [Video]. YouTube. https://www.youtube.com/watch?v=gH7vRekzx6o
Breast cancer statistics: How common is breast cancer?. Breast Cancer Statistics | How Common Is Breast Cancer? | American Cancer Society. (2023, January 12). https://www.cancer.org/cancer/types/breast-cancer/about/how-common-is-breast-cancer.html
Breast Self-Examination. (n.d.). Singapore Cancer Society. https://www.singaporecancersociety.org.sg/get-screened/breast-cancer/breast-self-examination.html
Britt, K. L., Cuzick, J., & Phillips, K.-A. (2020). Key steps for effective breast cancer prevention. Nature Reviews Cancer, 20(8), 417+. https://link.gale.com/apps/doc/A630441047/AONE?u=csufresno&sid=bookmark-AONE&xid=6b3b6579
Brown, C., Nevola, A., & Martin, B. C. (2018). Lack of Impact of the 2009 USPSTF Guidelines on Rates of Mammography Screening. Journal of women’s health (2002), 27(7), 875–884. https://doi.org/10.1089/jwh.2017.6425
BUPA Health UK. (2013, 6 August). How a Mammogram is Carried Out [Video]. YouTube. https://youtu.be/bPgz2-PcC2E?si=kF3uo5Mc5klOYKoB
Centers for Disease Control and Prevention. (2022, September 26). What is breast cancer? Centers for Disease Control and Prevention. Retrieved October 11, 2022, from https://www.cdc.gov/cancer/breast/basic_info/what-is-breast-cancer.htm
Hathaway, C., Paetsch, P., Li, Y., Wu, J., Asgarian, S., Parker, A., Welsh, A., Deverka, P., & Cohain, A. (2021). Association of Breast Cancer Screening Behaviors With Stage at Breast Cancer Diagnosis and Potential for Additive Multi-Cancer Detection via Liquid Biopsy Screening: A Claims-Based Study. Frontiers in oncology, 11, 688455. https://doi.org/10.3389/fonc.2021.688455
Lee, H. Y., Stange, M. J., & Ahluwalia, J. S. (2015). Breast cancer screening behaviors among Korean American immigrant women: findings from the Health Belief Model. Journal of transcultural nursing: official journal of the Transcultural Nursing Society, 26(5), 450–457. https://doi.org/10.1177/1043659614526457
Li, J., Humphreys, K., Ho, P. J., Eriksson, M., Darai-Ramqvist, E., Lindström, L. S., Hall, P., & Czene, K. (2018). Family History, Reproductive, and Lifestyle Risk Factors for Fibroadenoma and Breast Cancer. JNCI cancer spectrum, 2(3), pky051. https://doi.org/10.1093/jncics/pky051
Office of Disease Prevention and Health Promotion [OASH]. (n.d.). Increase the proportion of females who get screened for breast cancer – C‑05. Health People 2030. https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-females-who-get-screened-breast-cancer-c-05
Pitman, J. A., McGinty, G. B., Soman, R. R., Drotman, M. B., Reichman, M. B., & Arleo, E. K. (2017). Screening mammography for women in their 40s: The potential impact of the American Cancer Society and U.S. Preventive Services Task Force Breast Cancer Screening Recommendations. American Journal of Roentgenology, 209(3), 697–702. https://doi.org/10.2214/ajr.16.17759
Scott, J. (2022). Your Risk of Breast Cancer If Your Mother Had Breast Cancer. Verywell Health. https://www.verywellhealth.com/mother-daughter-breast-cancer-risk-430161
Smith, R.A., Manassaram-Baptiste, D., Brooks, D., Cokkinides, V., Doroshenk, M., Saslow, D., Wender, R.C. and Brawley, O.W. (2014), Cancer screening in the United States, 2014: A review of current American Cancer Society guidelines and current issues in cancer screening. CA A Cancer Journal for Clinicians, 64: 30-51. https://doi.org/10.3322/caac.21212
Tabár, L., Yen, A. M., Wu, W. Y., Chen, S. L., Chiu, S. Y., Fann, J. C., Ku, M. M., Smith, R. A., Duffy, S. W., & Chen, T. H. (2015). Insights from the breast cancer screening trials: how screening affects the natural history of breast cancer and implications for evaluating service screening programs. The breast journal, 21(1), 13–20. https://doi.org/10.1111/tbj.12354
What You’re Actually Feeling for During a Breast Self-Exam. (2021, January 11). Healthfully. https://healthfully.com/1012405-actually-feeling-during-breast-selfexam.html
Childhood Obesity

By: Mariana Aldana, Courtney Yang, Josian Zuniga
Introduction
In the United States, childhood obesity has become a global public health problem today. Statistics from the Centers of Disease Control and Prevention (CDC) show that about 1 in 5 children and adolescents are overweight and obese (CDC, 2022a). In addition, about 14.7 million children and adolescents between the ages of 2-19 years old are affected by childhood obesity (CDC, 2022b). Those who are mostly affected by childhood obesity are those in low-income minority groups such as Hispanics. The Hispanic population are considered one of the fastest growing populations and have the highest obesity rates (Salvo et al., 2019). Although obesity mostly affects Hispanics, it may occur in non-Hispanic Black children, non-Hispanic White children, and non-Hispanic Asian children (CDC, 2022b). Unfortunately, childhood obesity rates may increase due to family socioeconomic status. Families who are considered lower-income tend to have less adequate access to healthy foods and nearby parks for frequent exercise opportunities (Anderson et al., 2019). The built environment plays a large role on obesity rates and its impact particularly in children.
Although childhood obesity is on the rise, it is important to understand the population groups who are affected, risk factors, and preventative measures to lower the obesity rates. If obesity begins during early childhood and is not being recognized during its early stages, it can lead to poorer health problems during adolescence and adulthood. These health problems can consist of increased risk of high blood pressure, high cholesterol, type 2 diabetes, and asthma.
Risk Factors that Cause Childhood Obesity
Obesity occurs in most children who consume unhealthy/too much foods, have little physical activity, and get inadequate sleep. Children can be more susceptible to obesity due to parents/guardians and their perceptions of healthy foods and physical activity. Other major factors that can contribute to obesity may be due to genetics or specific types of illnesses and medications children take. Importantly, a child’s risk of obesity begins with their behavioral factors.
Preventive Measures
School is one environment where children spend most of their time. To limit childhood obesity rates, it is necessary that schools advocate and implement the importance of healthy eating. To help, schools can limit access to processed foods and increase the consumption of healthier snack/foods to lower obesity rates in children (Anderson et al., 2019). In addition, children need physical exercise everyday to stay healthy and active. Most schools implement physical activities such as PE activities at least once a week in addition to recess, lunch, and after school programs. To help decrease the childhood obesity rates, schools need to implement more PE activities everyday and not only once a week. School is quite important for children because when school is not in session, children can lack physical activity on a daily basis.
Parents and guardians can also help prevent childhood obesity from increasing. Parents and guardians should encourage children to develop healthy eating habits and to stay active on a daily basis. It can be quick and easy for parents or guardians to feed their children fast food, processed foods, and sugary foods frequently, but they should learn how to practice portion control on their children.
Portion Control- (One Serving)

Image was taken by: https://pixabay.com/vectors/my-plate-nutrition-nutrients-5336211/
Portion control is eating a healthy amount of certain foods. Portion control not only allows one to get the benefits of the nutrients in the food without overeating but also helps reach or maintain a healthy weight, digest food easier, control blood sugar levels, and stay energized throughout the day. If consumption intake increases, calories being consumed do as well. Unhealthy eating habits and patterns throughout early childhood is associated with nutrition-related noncommunicable diseases, such as obesity. Parents should surround their kids with healthy options at home and illustrate good nutrition to motivate healthy eating. A reason people eat too much at meals is due to eating what is seen on their plate (Gavin, 2022).
Dividing the plate into 4 sections is a method to understand one’s portion sizes. My Plate, by the U.S. Department of Agriculture, helps Americans with dietary guidelines and recommends the proper amount of food for individuals based on their age, sex, height, weight, and physical activity. The recommended portions for each food group is to visualize the plate divided into four sections. The four sections are made up of a quarter of protein (e.g., 1 ounce of meat or fish, 2 ounces of tofu, ¼ cup of cooked beans, 1 egg, 1 ounce of nuts or seeds), a quarter of grains (e.g., 1 slice of bread, ½ cup of cooked rice or cooked pasta), a quarter of fruits or 1 cup of 100% fruit juice and a quarter of raw or cooked vegetables (e.g., 2 cups of raw leafy salad greens) (Gavin, 2022). One can also include a dairy portion, such as 1 cup of milk of choice, yogurt, or 1 ½ ounces of cheese (Gavin, 2022).
Please visit: https://www.myplate.gov/eat-healthy/what-is-myplate for more information about portion control.
Physical Activity in Children
Youth who are physically active, have better cardiovascular strength, well built muscles and bones, and lower body fat compared to those who are not active. Children from the ages of 3–5 years should be physically active throughout the day. As to those who are aged 6–17 years need 60 minutes of physical activity at least daily (CDC, 2023). Some examples of physical activities that can encourage youth are hikes, bike rides, swimming, gardening, and sports. Physical wellness is not only important to the body but to the brain as well. It has been shown that physical activity helps with sleep and exercise is associated with improved quality of life and mood (Mahindru et al., 2023). Research shows that only 5 minutes of walking outside and interacting with nature, increases how one feels such as their self-esteem as well as their cognitive function (U.S. Department of the Interior, 2023).
Healthy People 2030 and Childhood Obesity
As with most public health issues, it is critical to be aligned in efforts and strategies to address childhood obesity across the United States. This is why it is crucial to incorporate national health objectives, like those from Healthy People 2030, into any health recommendations. One of the Healthy People 2030 Leading Health Indicators (LHIs) is to reduce the proportion of children and adolescents with obesity (Office of Disease Prevention and Health Promotion, 2023). An LHI is a subset of high priority Healthy People 2030 objectives. Unfortunately, this objective currently has little to no detectable change (Office of Disease Prevention and Health Promotion, 2023).
The prevention strategies recommended here were included for being culturally relevant to the target populations. For example, highlighting parental and familial values in the home is important when discussing health issues that disproportionately affect Hispanic households. Moreover, activities like walking/hiking, sports, and swimming are typically found in most communities. The key is to improve accessibility to healthy foods and green spaces, and continue to break down barriers that impede children from engaging with these activities in their daily life. These recommendations also aim to improve long-term health outcomes that include reducing diabetes and reducing pregnancy complications (Office of Disease Prevention and Health Promotion, 2023). Lastly, portion control and nutritious diets target other Healthy People 2030 objectives related to reducing sugar consumption and increasing healthcare counseling (Office of Disease Prevention and Health Promotion, 2023).
Conclusion
Overall, childhood obesity remains a pertinent issue in the United States that involves a complex variety of health determinants. This health issue is widespread across the U.S., however it disproportionately affects POC – especially Hispanics – and underserved communities. Parents and guardians, schools, education, youth recreation resources, and the built environment must all work in unison to ameliorate existing health disparities regarding childhood obesity. However, it is equally important that these actors are equipped with the proper resources to combat these issues. This means increasing accessibility, expanding sports programs, and promoting health education in underserved communities. By centering local and national efforts around Healthy People 2030 objectives it will help us close this gap and ensure the health of our future generations.
References
Anderson, P., Butcher, K. F., & Schanzenbach, D. W. (2019). Understanding Recent Trends in Childhood Obesity in the United States. Economics and Human Biology, 34, 16–25. https://doi.org/10.1016/j.ehb.2019.02.002
Centers for Disease Control and Prevention. (2022a). Childhood Overweight & Obesity. https://www.cdc.gov/obesity/childhood/index.html
Centers for Disease Control and Prevention. (2022b). Childhood Obesity Facts. https://www.cdc.gov/obesity/data/childhood.html
Centers for Disease Control and Prevention. (2023). Preventing Childhood Obesity: 5 Things Families Can Do. https://www.cdc.gov/nccdphp/dnpao/features/childhood-obesity/index.html
Gavin, M. L. (Ed.). (2022). Food portions: How much should I eat? (for teens) – nemours kidshealth. KidsHealth. https://kidshealth.org/en/teens/portion-size.html
Mahindru, A., Patil, P., & Agrawal, V. (2023, January 7). Role of physical activity on mental health and well-being: A Review. Cureus. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9902068/
Office of Disease Prevention and Health Promotion. (2023). Reduce the proportion of children and adolescents with obesity — NWS‑04. https://health.gov/healthypeople/objectives-and-data/browse-objectives/overweight-and-obesity/reduce-proportion-children-and-adolescents-obesity-nws-04
Salvo, D., Ranjit, N., Nielsen, A., Akhavan, N., & van den Berg, A. (2019). Characterizing Micro-scale Disparities in Childhood Obesity: Examining the Influence of Multilevel Factors on 4-Year Changes in BMI, Healthy Eating, and Physical Activity, Among a Cohort of Children Residing in Disadvantaged Urban Enclaves. Frontiers in Public Health, 7, 301–301. https://doi.org/10.3389/fpubh.2019.00301
U.S. Department of the Interior. (2023). Nature makes you… (U.S. National Park Service). National Parks Service. https://www.nps.gov/articles/naturesbenefits.htm#:~:text=Happier,lowers%20cortisol%20levels%20by%2015%25.
Image source: https://pixabay.com/illustrations/diet-nourishment-libra-1135819/
Health Communication
By Marlene Casarez, Andres Cruz, and Samantha Perez

The term “health communication” can refer to a variety of different activities, including healthcare professionals sharing information with their patients, public health officials holding public meetings, nonprofit organizations hosting forums, or government agencies giving press conferences (Health Communication, 2020). It is distributed using a wide variety of channels and can take the form of a number of different types of media, such as articles, videos, pamphlets, and educational events (e.g., social media, radio, websites, and television) (Health Communication, 2020).
The Importance of Health Communication
It is essential to one’s health and well-being to have effective communication regarding health. The Healthy People 2030 initiative places a strong emphasis on enhancing health communication in the hopes of making it simpler for individuals to comprehend and act upon health information (Health Communication – Healthy People 2030 | Health.Gov, n.d.).
The information and messages that pertain to health are frequently overly complicated, which makes them difficult to comprehend and difficult to apply. People are able to make more informed decisions regarding their health when their health care providers communicate with them clearly, use methods such as teach-back, and participate in shared decision-making (Health Communication – Healthy People 2030 | Health.Gov, n.d.) These strategies have the potential to help improve outcomes, particularly for specific groups, such as people who have limited health literacy skills or speak English as a second language (Health Communication – Healthy People 2030 | Health.Gov, n.d.).
It is also essential to the process of improving health and well-being to ensure that electronic health information is simple to understand and use. In addition, news organizations and health departments are able to improve public health and safety by employing efficient communication strategies. For instance, they can make information that is both complete and actionable available to the public and engage in social marketing (Health Communication – Healthy People 2030 | Health.Gov, n.d.).
Characteristics of Effective Health Communication
Because effective health communications can have a real impact, public health professionals need to think about how to reach an audience while taking into account the various ways in which individuals process and receive information. Understanding an audience’s beliefs about how a health issue is relevant to them, for example, can help professionals craft more effective health messages (Health Communication, 2020).
According to Tulane University School of Public Health, the most effective health communications are:
- Not only relevant and accurate but also unbiased and nonjudgmental
- Culturally competent (taking into consideration the differences in the audience’s educational levels and religious and cultural beliefs)
- Easily accessible in terms of location, language, and format
- Actionable (providing resources and instructions that allow people to act on advice given)
- Available to as many people who need the information as possible
- Balanced, recognizing both risks and benefits
(Health Communication, 2020)
In the scope of public health and health promotion, there is a growing interest and understanding that audience insight is essential in defining and testing communication interventions. Research has demonstrated that messages can be processed more thoroughly if the content is specialized to a person’s cognitive, affective, and motivational behaviors. These behaviors depend on an individual’s cultural background and understanding. This tailoring of messages is crucial not only for health promotional practices but also important for helping individuals make medical decisions (Betsch, 2016). With the growing technological applications, it is also becoming easier for health messages to be accessible. An example would be during the time of the COVID-19 pandemic when countries around the world took various approaches to disseminate information to the population about the disease. An international study analyzed and compared the health communication approaches of the United States, Sweden, and Italy. The study concluded that while the countries worked with their respective government organizations to disseminate information, the United States did not often tailor the messages to particular social groups who were at risk, such as pregnant women and the homeless population (Tagliacozzo, 2021). This highlights that even national health communication should constantly be improved and adapted from its shortcomings.
Health Education
Health education is about teaching targeted audiences about a wide variety of health topics in order for them to take the steps necessary to maintain their overall health. Education can happen in many settings, such as schools, and can include a curriculum based on personal experiences. For example, a campaign to raise awareness of the risk of suicide may be implemented in schools (Health Communication, 2020). In addition, medical and dental offices may show videos or distribute pamphlets regarding the prevention and treatment of colon cancer and proper dental hygiene, respectively. In each of these situations, the information assists in raising awareness among the audience, which in turn prepares people to make decisions that are better for their health (Health Communication, 2020). Ideally, the information communicated by health educators should be actionable information that the target audience can apply to their daily lives. In turn leading to the adoption of the desired behaviors that lend to more favorable health outcomes. Making use of the appropriate channels and models derived from communication theory can equip health educators with the tools necessary to reach their target audiences effectively. Models such as Rosenstock’s Health Belief Model is commonly used to understand health behaviors while Bettman’s Consumer Information Processing Model can explain the capacity individuals have to process information.
Health Advocacy
The goal of health advocacy is to improve people’s health by ensuring their access to appropriate medical care, promoting policies and procedures that improve the quality of healthcare, while working to simplify the process of navigating the healthcare system (Health Communication, 2020). When it comes to locating qualified physicians, both individuals and communities may experience a sense of helplessness (Health Communication, 2020). They might not be aware of the proper procedures for verifying the information on medical bills (Health Communication, 2020). The goal of health advocacy is to develop initiatives and resources that can help address problems of this nature (Health Communication, 2020). Subsequently health advocay’s goal can only be achieved through effective health communication. Especially in regards to navigation of the health care system where one’s level of health literacy can directly correlate to their success during this process. Health literacy refers to the degree of which an individual has the capacity to find, understand, and use health information/services to inform their health decisions (HRSA, 2022). One approach to better everyone’s access and ability to navigate the healthcare system may consist of improving their level of health literacy through employing effective health communication strategies. Public Health practitioners can also tailor their health information messages to reach segments of the population facing the most dire health disparities. This would require the shared information to be appropriate for the target audience so that they can understand and apply that health information effectively.
References
Betsch, C., Böhm, R., Airhihenbuwa, C. O., Butler, R., Chapman, G. B., Haase, N., Herrmann, B., Igarashi, T., Kitayama, S., Korn, L., Nurm, Ü.-K., Rohrmann, B., Rothman, A. J., Shavitt, S., Updegraff, J. A., & Uskul, A. K. (2016). Improving Medical Decision Making and Health Promotion through Culture-Sensitive Health Communication: An Agenda for Science and Practice. Medical Decision Making, 36(7), 811–833.
https://doi.org/10.1177/0272989X15600434
Health communication: Effective strategies | tulane university. (2020, September 25).
Health Communication—Healthy People 2030 | health.gov. (n.d.). Retrieved February 14, 2023, from https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-communication
Tagliacozzo, S., Albrecht, F., & Ganapati, N. E. (2021). International Perspectives on COVID-19 Communication Ecologies: Public Health Agencies’ Online Communication in Italy, Sweden, and the United States. American Behavioral Scientist, 65(7), 934–955. https://doi.org/10.1177/0002764221992832
(Health Communication Scholars | Moody College of Communication, n.d.)
Malikhao P. (2020). Health Communication: Approaches, Strategies, and Ways to Sustainability on Health or Health for All. Handbook of Communication for Development and Social Change, 1015–1037. https://doi.org/10.1007/978-981-15-2014-3_137
Rimal, R. N., & Lapinski, M. K. (2009). Why health communication is important in public health. Bulletin of the World Health Organization, 87(4), 247–247a. https://doi.org/10.2471/blt.08.056713
Ishikawa, H., & Kiuchi, T. (2010). Health literacy and health communication. BioPsychoSocial medicine, 4, 18. https://doi.org/10.1186/1751-0759-4-18
HRSA. (2022) Health Literacy. Health Resources & Services Administration. Retrieved: https://www.hrsa.gov/about/organization/bureaus/ohe/health-literacy#:~:text=Personal%20health%20literacy%20is%20the,actions%20for%20themselves%20and%20others.
Tobacco Use Among Children
By: Ruby Ramos, Josh Esperanzate, & Marlene Casarez

Image was taken from https://pixabay.com/
Key Facts About Tobacco Use Among Children
Nearly 2,500 children under the age of 18 have their first experience with a cigarette every single day, and more than 400 of those children will go on to become new, habitual daily smokers (Association, n.d.). At some point in the future, half of them will pass away as a direct result of their habit (Association, n.d.). People who start smoking at a younger age are more likely to acquire a strong addiction to nicotine than those who don’t start smoking until much later in life (Association, n.d.). The majority of young people who have smoked at least 100 cigarettes in their lifetime claim that they want to quit smoking but are unable to do it on their own (Association, n.d.). This is especially true of those who have smoked more than 50 cigarettes in their lives (Association, n.d.). If current patterns of tobacco use continue, it is anticipated that 5.6 million of today’s children and adolescents under the age of 18 will die prematurely from an illness associated with smoking in the future (Association, n.d.).
If the current incidence of cigarette smoking among young people in this country remains unchanged, an estimated 5.6 million American children and teenagers under the age of 18 will experience a premature death due to a disease that is associated with smoking (CDCTobaccoFree, 2022). That accounts for approximately 1 out of every 13 young Americans under the age of 17 who are still living in the United States today (CDCTobaccoFree, 2022). According to the CDC, In the year 2022, approximately one out of every hundred in middle school (1.0% of the student body) disclosed that they had smoked cigarettes within the preceding 30 days (CDCTobaccoFree, 2022). In 2022, roughly two out of every one hundred high school students (2.0%) claimed that they had smoked cigarettes within the preceding thirty days (CDCTobaccoFree, 2022).

(CDCTobaccoFree, 2022)
Tobacco Prevention Efforts
The detrimental consequences of smoking reach practically every organ in the body, making smokers more vulnerable to various disorders and lowering their overall health quality. The youth is a target population for flavored tobacco products as mentioned by the Centers for Disease Control and Prevention (2021). According to the Centers for Disease Control and Prevention (2021), the Office on Smoking and Health (OSH) assists states and communities in the process of implementing tobacco control activities by promoting national and local campaigns and events, linking to state and community resources, providing suggestions, and compiling data. The National and State Tobacco Control Program (NTCP), established by the Office of Smoking and Health in 1999 to support and coordinate national efforts to decrease tobacco-related illnesses and deaths, was meant to support and coordinate national actions (CDC, 2021). Tobacco prevention activities in state and territory health departments are eligible for financing and technical assistance under this program. The program offers to fund other programs that aim to reduce tobacco use or their efforts in providing education on tobacco to their communities. Education is essential when trying to reduce tobacco use because many people are unaware of the consequences. The goals of National and State Tobacco Control Programs include:
- Reduce or eliminate exposure to ambient cigarette smoke.
- Increase health equity by determining the causes of health disparities and inequalities caused by commercial tobacco products and working to eliminate such disparities and inequalities.
- End the initiation practice among young people of all ages, particularly children and teens.
- Everyone, including children and adults, should be encouraged to break the habit of smoking. Increase health equity by determining the causes of health disparities and inequalities caused by commercial tobacco products and working to eliminate such disparities and inequalities.
(CDC, 2021)
The mission of the California Tobacco Control Program, which is a program of the California Department of Public Health, is to create an atmosphere free of tobacco use through supervising health programs, services, and activities at the state and the local level (California Department of Public Health, 2023). The mission of the California Tobacco Control Program is to change the social norms associated with tobacco use. This will be accomplished by “indirectly influencing current and potential future tobacco users by creating a social milieu and legal climate in which tobacco becomes less desirable, less acceptable, and less accessible” (California Department of Public Health, 2023). The California Tobacco Control Program also offers different grants and funding that local organizations can apply for that meet the needs or have similar missions to the CTCP. They fund tobacco prevention programs in order to impact a variety of people. This increases the chance of local prevention programs that serve impacted communities applying for these grants and making changes within their community. Some of the priorities that the California Tobacco Control Program and similar prevention programs that they may provide funding for should have are:
- Reducing the impact of factors that encourage tobacco use
- Reducing exposure to secondhand smoke, tobacco smoke residue, other tobacco products, and tobacco waste
- Making tobacco more challenging to get, policies to enforce the limit of tobacco sell
- Promoting tobacco cessation
(California Department of Public Health, 2023)
Tobacco Usage in Healthy People 2030
In regards to Healthy People 2030, goals established for smoking amongst adolescents show a wide variety of target areas. There is the establishment of the past hurdles in tobacco usage, such as the status of cigar and cigarette usage amongst adolescents. They were established as prominent trends in the past but are still shown to have presence amongst the adolescent population. Healthy People 2030 also highlights that adults who are current cigarette smokers were found to have most likely started before the age of 18 (Office of Disease Prevention and Health Promotion, 2023). However, the newest trends in tobacco usage were shown to be focused on e-cigarettes and marketing directed towards a younger audience. Healthy People 2030 has found that the rise of e-cigarette devices and the marketing towards a younger audience has allowed the tobacco usage prevalence in the United States to remain at a constant. This constancy in the tobacco spaces is contrasted directly with the visible decrease in traditional tobacco use such as cigars and cigarettes.
Conclusion
With these trends in mind, the goals that Healthy People 2030 set out have shown a mixed set of results. Some goals such as decreasing the levels of cigarette usage (TU-06) or smokeless tobacco usage (TU-08) were considered met or exceeded by Healthy People 2030 (Office of Disease Prevention and Health Promotion, 2023). Goals focused on reduction of cigar smoking (TU-07) and reducing adolescents getting into smoking (TU-09) have shown improvements in recent years. One goal that Healthy People 2030 has found to be ‘getting worse’ was the goal of reducing the amount of adolescents that are currently using tobacco products as a whole (TU-04). While earlier attempts have been focused on reducing prevalence of traditional forms of tobacco usage, the current health trends need to be focused more on policy and attempting to reduce modern forms of tobacco consumption (Office of Disease Prevention and Health Promotion, 2023).
References
Association, A. L. (n.d.). Tobacco use among children and teens. Retrieved April 12, 2023, from https://www.lung.org/quit-smoking/smoking-facts/tobacco-use-among-children
California Department of Public Health. (2023, February 23). CALIFORNIA TOBACCO CONTROL
BRANCH. Retrieved April 12, 2023, from https://www.cdph.ca.gov/Programs/CCDPHP/DCDIC/CTCB/Pages/Welcome.aspx#3
CDCTobaccoFree. (2022, November 9). Youth and tobacco use. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/index.htm
Centers for Disease Control and Prevention. (2021, November 24). National and State Tobacco Control
Program. Centers for Disease Control and Prevention. Retrieved April 12, 2023, from https://www.cdc.gov/tobacco/stateandcommunity/tobacco-control/index.htm
Office of Disease Prevention and Health Promotion. (2023). Reduce current cigarette smoking in adolescents — TU‑06. https://health.gov/healthypeople/objectives-and-data/browse-objectives/tobacco-use/reduce-current-cigarette-smoking-adolescents-tu-06
Office of Disease Prevention and Health Promotion. (2023). Reduce current tobacco use in adolescents — TU‑04. https://health.gov/healthypeople/objectives-and-data/browse-objectives/tobacco-use/reduce-current-tobacco-use-adolescents-tu-04
Office of Disease Prevention and Health Promotion. (2023). Reduce the proportion of adolescents exposed to tobacco marketing — TU‑22. https://health.gov/healthypeople/objectives-and-data/browse-objectives/tobacco-use/reduce-proportion-adolescents-exposed-tobacco-marketing-tu-22
Environmental Health
By: Andres Cruz, Naomi Hematillake, Stephany Roldan

Introduction
According to the American Public Health Association (APHA), environmental health is a subset of public health that is defined by an individual’s environmental impact (Environmental Health, n.d.). This impact includes their influence on sources such as agriculture, air, water, and more (Environmental Health, n.d.). This topic is especially significant when considering the social determinants of health. Research shows that an individual’s race, socioeconomic status, education, age, and more impact their environmental health outcomes (Schulz & Northridge, 2004). A conceptual model illustrating the social determinants of health by Schulz & Northridge identifies four categories of environmental health that influence the social determinants: Fundamental, intermediate, proximate, and health and well-being (Schulz & Northridge, 2004). The fundamental level refers to the macro level of environmental impact influenced by climate, historical events and more (Schulz & Northridge, 2004). The intermediate level refers to the community level of environmental impact which is influenced by policies and zoning regulations (Schulz & Northridge, 2004). The proximate level refers to the interpersonal factors such as neighborhood, health behaviors and more (Schulz & Northridge, 2004). Finally, health and wellbeing are the individual factors that impact the environment (Schulz & Northridge, 2004).
The natural environment is coded under the fundamental level, which includes macrosocial factors such as historical impacts, legality, human rights, racism, and social justice. These factors further lead to social inequalities, which impact one’s education, distribution of wealth, and more (Schulz & Northridge, 2004). For example, race has a significant impact on environmental health. Riddell and colleagues’ 2021 study on the impacts of traffic-related air pollutants among Asian, white, Latina, and Black women in Oakland and San Jose, California, show that Black and Latina’s women have disproportionately higher rates of preterm birth than Asian and white women. One reason may be that their general environment was formed due to historical racism and redlining (Riddell et al., 2021). This research suggests that exploring the factors related to environmental health and its impact on global and national populations is essential to promote health for all.
Health Effects of Environmental Hazards
Several environmental health issues, including water and air pollution, extreme temperatures, and chemical exposures, can all be detrimental to human health, contributing to severe and minor conditions such as cancer and heat exhaustion. According to the Pan American Health Organization (PAHO), approximately 83 million people still lack adequate sanitation systems, with 15.6 million still practicing open defecation and 28 million lacking access to improved sources of safe drinking water, resulting in approximately 30,000 preventable deaths each year; additionally, hazardous chemical risks, such as exposure to toxic pesticides, lead, and mercury, disproportionately affect children and adolescents. Toxic chemical exposure can cause persistent, often irreversible problems such as neurodevelopmental abnormalities, congenital deformities, and endocrine-disrupting diseases (Environmental Determinants of Health – Paho/Who | Pan American Health Organization, n.d.).
Finally, environmental changes such as climate change are increasingly negatively impacting people’s health and well-being by disturbing global physical, biological, and ecological systems. Extreme weather events have exacerbated food shortages, air pollution, access to clean water, population migration, and vector-borne disease transmission patterns (Environmental Determinants of Health – Paho/Who | Pan American Health Organization, n.d.). These environmental issues may increase the incidence of respiratory, cardiovascular, and infectious diseases, as well as injuries, heat stress, and mental health problems.
Healthy People 2030
Healthy People 2030 identifies national objectives created by the United States Department of Health and Human Services to improve the health of all Americans. Healthy People 2030 seeks to improve health and prevent disease by creating measurable objectives and targets to improve health outcomes in various areas, including environmental health (About Healthy People 2030 – Healthy People 2030. n.d.).
Environmental health is essential to public health because it relates to the manner in which the environment influences human health. This encompasses air and water quality, hazardous waste management, food safety, and climate change. The Healthy People 2030 plan includes various environmental health objectives, including:
- Reduce the number of days people are exposed to unhealthy air (EH‑01): This objective seeks to decrease the number of individuals exposed to hazardous environmental pollutants including reducing exposure to various contaminants such as lead, air pollution, and pesticides. This objective also seeks to raise public awareness of environmental risks and encourage the adoption of protective behaviors (Reduce the Number of Days People Are Exposed to Unhealthy Air — EH‑01 – Healthy People 2030. n.d.).
- Increase the proportion of people whose water supply meets Safe Drinking Water Act regulations (EH‑03): This objective aims to improve Americans’ equitable access to safe and clean drinking water. This involves increasing access to water testing and treatment services and increasing the number of people who obtain their drinking water from systems that meet federal and state water quality requirements (Increase the Proportion of People Whose Water Supply Meets Safe Drinking Water Act Regulations — EH‑03 – Healthy People 2030. n.d.).
- Reduce the number of toxic pollutants released into the environment (EH‑06): This objective aims to mitigate the adverse health consequences of climate change, including heat-related illnesses, respiratory illnesses, and vector-borne diseases. This includes promoting strategies to reduce greenhouse gas emissions, adapting to the effects of climate change, and raising public awareness of the health impacts of climate change (Reduce the Amount of Toxic Pollutants Released into the Environment — EH‑06 – Healthy People 2030. n.d.).
The objectives are intended to be measurable and attainable within the following decade. The practical application of these objectives are described above. By pursuing these objectives, the Healthy People 2030 initiative attempts to improve environmental health and promote the health and well-being of all Americans (Brusseau et al., 2019).

Solutions to Environmental Health Issues
Different parts of the globe suffer from different environmental challenges, for some it’s potable water while for others climate change has brought more extreme natural disasters such as record-breaking floods or wildfires. Thus a well informed and tailored approach is often required to address the environmental health issues of any given region or population. If air pollution is the issue then policies such as the Clean Air Act from the EPA have long since regulated the emissions of industrial sources (EPA, 2023). If climate change has brought about more severe natural disasters such as flooding or wildfires then efforts can be focused towards land management and emergency preparedness. For example, reinforcing water barriers such as levees and early warning systems can mitigate flood disasters by giving people more time to evacuate safely. In regards to water sanitation, policies such as the Clean Water Act regulate water pollution and the water quality of the nation’s waterways (EPA, 2023).
Therefore the solution to environmental health issues lies within environmental health advocacy that leads to appropriate policies and interventions. Pathways to this may come in the form of environmental research/monitoring, education, information dissemination, and environmental conservation. As populations grow, so do many of the aforementioned environmental health issues. Raising awareness and closely monitoring the natural world around us will help maintain the health of ourselves through the health of our environment.
References
About Healthy People 2030—Healthy People 2030. Health.gov. (n.d.). Retrieved April 12, 2023, from https://health.gov/healthypeople/about
Brusseau, M. L., Ramirez-Andreotta, M., Pepper, I. L., & Maximillian, J. (2019). Environmental impacts on human health and well-being. In Environmental and Pollution Science (pp. 477–499). Elsevier. https://doi.org/10.1016/B978-0-12-814719-1.00026-4
Environmental determinants of health—Paho/who | pan american health organization. (n.d.). Retrieved April 12, 2023, from https://www.paho.org/en/topics/environmental-determinants-health
Environmental health. (n.d.). Retrieved April 9, 2023, from https://www.apha.org/topics-and-issues/environmental-health
Environmental Protection Agency. (n.d.). EPA. Retrieved April 10, 2023, from https://www.epa.gov/
Home. The Global Climate and Health Alliance. (2023, February 9). Retrieved April 10, 2023, from https://climateandhealthalliance.org/
Increase the proportion of people whose water supply meets Safe Drinking Water Act regulations—EH‑03—Healthy People 2030 | health.gov. (n.d.). Retrieved April 12, 2023, from https://health.gov/healthypeople/objectives-and-data/browse-objectives/environmental-health/increase-proportion-people-whose-water-supply-meets-safe-drinking-water-act-regulations-eh-03
Reduce the amount of toxic pollutants released into the environment—EH‑06—Healthy People 2030 | health.gov. (n.d.). Retrieved April 12, 2023, from https://health.gov/healthypeople/objectives-and-data/browse-objectives/environmental-health/reduce-amount-toxic-pollutants-released-environment-eh-06
Reduce the number of days people are exposed to unhealthy air—EH‑01—Healthy People 2030 | health.gov. (n.d.). Retrieved April 12, 2023, from https://health.gov/healthypeople/objectives-and-data/browse-objectives/environmental-health/reduce-number-days-people-are-exposed-unhealthy-air-eh-01
Riddell, C. A., Goin, D. E., Morello-Frosch, R., Apte, J. S., Glymour, M. M., Torres, J. M., & Casey, J. A. (2022). Hyper-localized measures of air pollution and risk of preterm birth in Oakland and San Jose, California. International journal of epidemiology, 50(6), 1875–1885. https://doi.org/10.1093/ije/dyab097
Schulz, & Northridge, M. E. (2004). Social Determinants of Health: Implications for Environmental Health Promotion. Health Education & Behavior : the Official Publication of the Society for Public Health Education., 31(4), 455–471. https://doi.org/10.1177/1090198104265598
U.S. Department of Health and Human Services. (n.d.). National Institute of Environmental Health Sciences (NIEHS). National Institute of Environmental Health Sciences. Retrieved April 10, 2023, from https://www.niehs.nih.gov/

